A survey on personalized medicine was conducted by P1-MUI and P8-REGIONH to raise awareness of patients and public. To investigate understanding and interest of the public/patients towards precision medicine a questionnaire with five questions (Q1 – Q5) was presented at a patient symposium to 54 Austrian CKD patients and their relatives and to 124 Danish diabetes outpatients. A combined analysis of the results provided general information on patient perceptions but also allowed a comparison between two European Union countries. A chi-square test (Q1, Q3, Q4, Q5) evaluated the significant association between Austria and Denmark, Q2 was evaluated using the Wilcoxon test. The results are shown in Figure 1 to Figure 5.
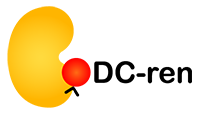
Q1:
Have you ever heard of personalized medicine before this event?
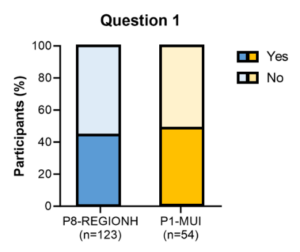
Figure 1: Result of the patient survey on precision medicine for Q1.
Q2:
What is your personal opinion on personalized medicine?
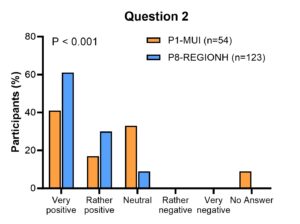
Figure 2: Result of the patient survey on precision medicine for Q2.
Q3:
Imagine the following situation: You are healthy and your doctor will offer you a test that predicts whether you will develop a very rare (only one person in 10,000) but fatal disease in the next ten years. Unfortunately, there is no treatment for this disease once it has broken out. However, it is possible to significantly delay the onset of the disease with a drug (e.g. by ten years). The drug has massive side effects. You know from the test that it covers everyone who will fall ill. However, it is also positive (i.e. false) in 30% of persons who do not fall ill. In these people, the drug would of course have no protective effect, only a negative one.
Figure 3: Result of the patient survey on precision medicine for Q3.
Q4:
You suffer from a chronic kidney disease. There is a completely new test that can predict with 80 % certainty whether you will respond particularly well to a certain medication. The test is complicated, based on artificial intelligence methods, and neither you nor your doctor understand how it works.
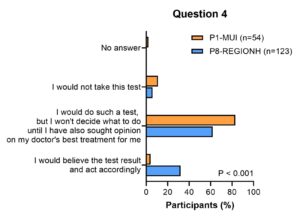
Figure 4: Results of the patient survey on precision medicine for Q4.
Q5:
Optimal personalized diagnostics naturally require the collection of very personal data. If this data is anonymized (i.e. it is no longer possible to trace the origin of the data) who is most likely to get access from your point of view (multiple answers possible)?
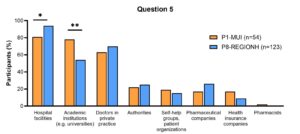
Figure 5: Result of the patient survey on precision medicine for Q5.
Overall, high interest was monitored in both countries. A positive attitude towards personalized medicine was observed, which was significantly higher in Denmark (Figure 3, Q2; P˂0,001). Many participants expressed great confidence in the treatment decisions based on personalized medicine tools, as long as decisions could be discussed with treating health care professionals (Figure 5). There was a significant higher level of willingness of the Danish participants to allow the use of personal data for optimal personalized diagnostics in hospital facilities, CKD patients from Austria significantly preferred academic institutions (Figure 6, Q5; P˂0,01 and P˂0,05). No other significant differences between the groups were present.
A comparison of the expert and patient survey shows that many patients and specialists expect benefits from precision medicine and have a positive attitude towards it. However, professionals seem to perceive more risks, in particular the lack of evidence for the accuracy of the tests and the effectiveness of the treatments. The experts believe that their recommendations to use AI tools for risk assessment are highly accepted by patients, although no rational explanations are possible. The results of the patient survey show that the opinion of the attending physician is highly valued, albeit to a somewhat lesser extent than the physicians assume.